In this series, we’ve discussed:
- Provider Adoption
- Access to Specialty Care
- Clinical Quality
- Patient Benefits
- Practice Performance & Cost Savings
In this blog, we will focus on cost savings delivered from eConsult program. Let’s start by reviewing a few challenges to effective care and practice success.
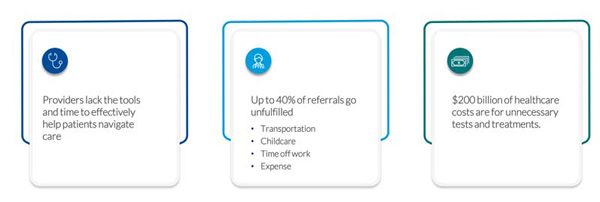
Primary care providers lack the tools and time to help patients navigate care. The average PCP sees between 10-20 patients per day. If you own your practice, you likely see more than 20 patients daily. Patient care is their goal. Adding new technology adds to their workload.
At the same time, not getting specialist advice for the patient is creating additional work for PCPs. More than 40% of referrals never get scheduled. That means more work for the PCP as patients boomerang back to the primary care setting with the same untreated condition.
$200 billion, or 25% of our healthcare costs, are for unnecessary tests and treatments. This figure doesn’t include unnecessary emergency room visits, multiple visits to your clinic because a patient can’t get an appointment quickly or increased cost of care due to untreated conditions. After all, your patients never made that specialist appointment.
Challenges to Effective Care and Practice Success
How do eConsults solve these challenges? eConsults are proven to reduce specialty care costs for patients, providers and payers. eConsults also support value-based care in tangible and practical ways. They create a path to faster diagnosis and treatment, improve or eliminate wait times for specialists’ visits, increase access to sub-specialties, and minimize worsened health outcomes resulting from delayed patient care. At-risk practices see tremendous cost savings by eliminating unnecessary specialty visits, reducing ED use and preventing hospital admissions and readmission.
But once you have an eConsult program in place, how do you measure the value of eConsults to your practice?
Solutions for Effective Care and Practice Success

eConsults drive cost savings for your practices by:
- Replacing referrals
- Eliminating unnecessary testing
- Reducing emergency room visits
- Avoiding hospital readmissions
An eConsult that avoids a specialty referral results in:
- 3 avoided specialty visits, which is the average number of appointments needed to diagnose and treat a patient.
- Each specialty visit costs approximately $300. The avoided visit savings to an at-risk practice is $900.
Approximately 20% of patients have non-clinically indicated duplicate testing when referred to a specialist, which can be avoided using eConsults. Averaged per patient, unnecessary tests and lab work cost about $85. Accounting for the cost of the eConsult, the total savings is $885.
Practice Cost Savings from an Avoided Specialty Referral

This example reflects the cost savings for a typical patient. What if your patient is at risk of visiting the ED, was recently discharged from the hospital, or takes multiple prescriptions? There are more than 139 million emergency room visits each year. The Agency for Healthcare Research and Quality estimates that between 13-27% of these visits could be managed outside of the ED. Using a conservative 13%, 18 million ED visits could be avoided annually. Across the average patient panel, 137 ED visits could be managed in the primary care setting. A savings of $157,000. This is the single biggest area of potential cost savings for a primary care practice, followed by hospital readmissions.
A single hospital readmission costs about $15,000. Fourteen percent of patients are readmitted to the hospital within 30 days, and 27% of those readmissions are avoidable. This translates to about seven patient readmissions or approximately $105,000 annually within the average PCP patient panel. Now, these calculations are dependent on the makeup of your patient population. If you have a higher percentage of elderly patients or manage a high number of chronic conditions or comorbidities — this number could be higher.
Additional Practice Cost Savings
ED Visits
- $1,150 per readmission
- 137 ED visits per provider panel
- 13% of ED visits are avoidable
Hospital Readmission
- $15,000 per readmission
- 14% of patients are readmitted
- 27% of these are avoidable
Adverse Drug Events
- $9,900 average cost per ADE
- ~1% of patients will experience an ADE annually
On the other hand, more than 56% of all patients will experience a drug-related error. Errors related to diagnosis were the most common reason. Not all errors will result in an Adverse Drug Event (ADE), but a surprising number occur each year. The result is more than 1.3 million emergency visits and 350,000 hospitalizations. The CDC reports blood thinners, diabetes, seizure and heart medications are most likely to cause an ADE. The cost of an ADE averages $9,900. While only 1% of the population will experience an ADE each year, patients recently discharged from the ED or inpatient care are more likely to experience an ADE:
- Only 10% of elderly patients will be discharged on the same medication that they were admitted to hospital on.
- 60% of patients will have three or more medicines changed during a hospital stay
- 28–40% of medications are stopped within the hospital
- 45% of medicines prescribed at discharge are new
Requesting a medication review via eConsult following a hospital discharge could save your practice a tremendous amount of money. The typical patient panel will experience four ADEs each year, costing your practice $9,900.
