Patient access management is currently a high priority due to a short supply of providers. Merritt Hawkins reports that the average wait time for a specialist appointment is 26 days. In numerous metro areas and specialties, patient wait times exceed 100 days. With a flood of patients overdue for care, states are turning to nurse practitioners (NPs) and physician assistants (PAs) to improve access to primary care.
What’s Causing the Healthcare Staff Shortages?
According to the U.S. Bureau of Labor Statistics, of the 4.5 million people who quit their jobs in November 2021, 6.4% were healthcare and social assistance workers. That’s one of the highest quit rates in any industry, second only to accommodation and food services. Burnout rates among healthcare workers are also skyrocketing. Major news outlets have reported that many doctors are exiting the field completely.
This exodus comes at a time of high appointment demand, with rebounding patient volumes in hospitals and health systems from people who put off care during the pandemic. As healthcare providers leave the workforce, the ability of APs to provide unrestricted care is expanding to fill the gap.
In 2020, California tackled the primary care provider shortage by passing a law to allow nurse practitioners to practice without physician supervision after meeting certain criteria. The timely passage of this legislation will help address an expected shortage of more than 4,000 primary care physicians in the state and reduce the number of patients waiting for care because of the pandemic.
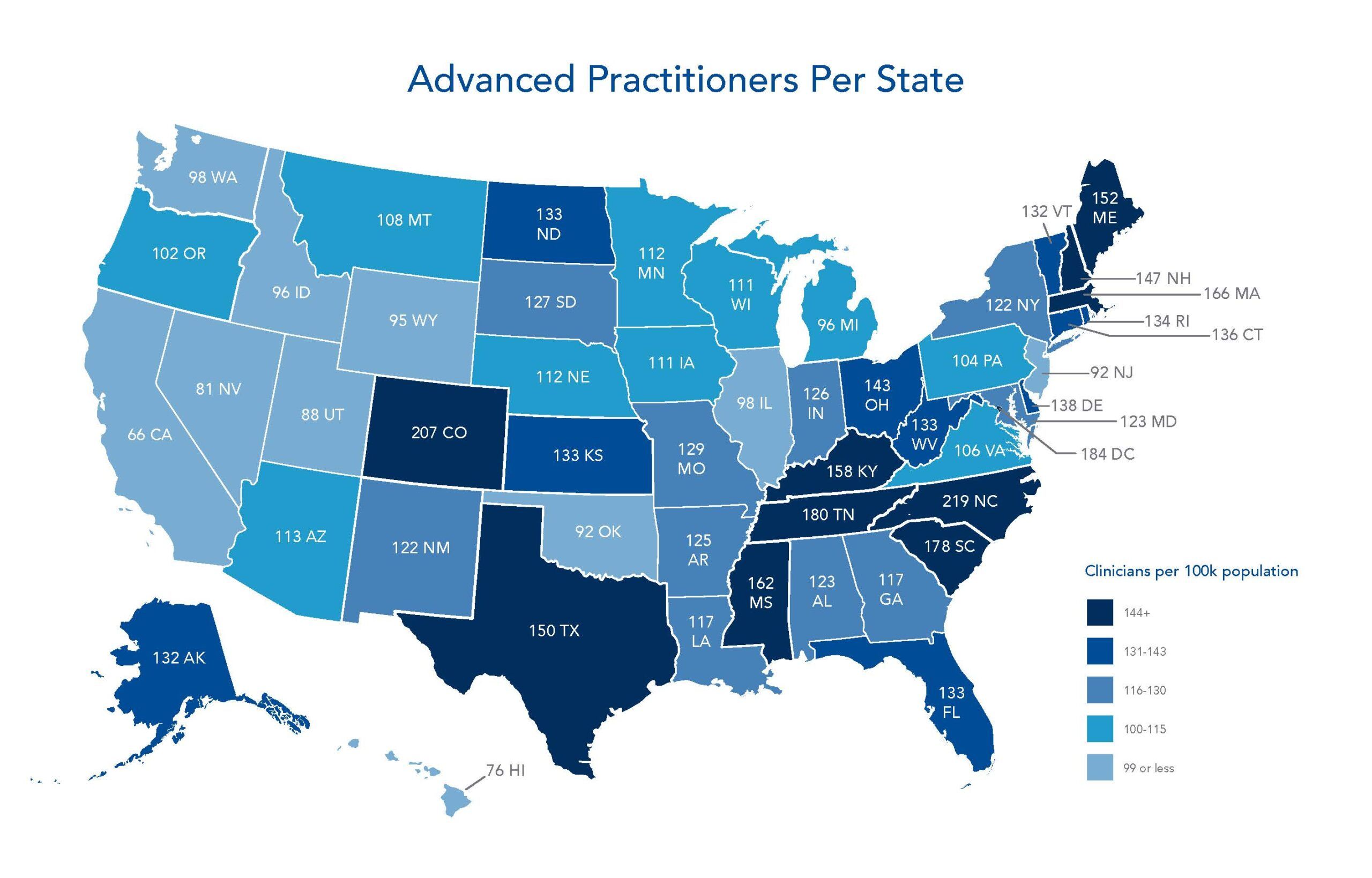
Advanced practitioners (APs) in 25 states and the District of Columbia care for patients with minimal limitation or supervision by physicians. In these States, NPs and PAs are supervised by a physician for a defined period of time before being able to practice independently. In states that limit the ability of APs to provide care, physician supervision is generally required for the duration of the AP’s career.
A Crisis Remains
In an overburdened system, physicians are focused on providing care to patients, leaving them with little time to supervise APs or coordinate with specialists. According to the U.S. Bureau of Labor Statistics, of the 4.5 million people who quit their jobs in November 2021, 6.4% were healthcare and social assistance workers. That’s one of the highest quit rates in any industry, second only to accommodation and food services.
Covid-19 is causing burnout rates among healthcare workers to skyrocket. Major news outlets have reported that many doctors are exiting the field completely. Nurses and other healthcare professionals are either quitting or threatening to quit at alarming rates, leaving those that remain with a larger burden of patients to care for.
While NPs and PAs are poised to alleviate the crisis in staffing, APs must be supervised by a physician in 25 states, and newly licensed APs must remain under the supervision of a physician in the states that allow independent mid-level practice.
How can clinics and practices minimize the time required to supervise APs? Can APs expand their experience and scope of practice to care for more complex patients? Yes.
With the help of eConsults:
- Mid-levels receive specialist insight to develop an appropriate care plan.
- Supervising physicians gain confidence in these care plans with the support of specialist advice.
- Patient access management and care improve as specialty care is delivered quickly, and face-to-face specialist visits are avoided.
Using eConsult technology, advanced practitioners can help primary care physicians manage patients who need specialty care, relieving the burden on providers while increasing the quality of care for patients. Mid-level providers, including nurse practitioners and physician assistants, can use eConsults to help patients gain access to specialists, reduce wait times for specialty care, and provide game-changing support to both PCPs and specialists.
Easing Patient Access Management Challenges
Research has shown that the quality of primary care provided by NPs and PAs is similar to that of physicians. However, APs have often focused on caring for patients with less complicated conditions and fewer patients with comorbidities.
With the growing demand for care and a shrinking pool of providers, APs are shouldering more responsibility for complex care. Telemedicine technology that enables these practitioners to connect with specialty physicians without requiring a face-to-face meeting or escalation to the on-site primary care physician is invaluable.
With eConsults, providers can consult a specialist about a patient’s condition or chief complaint. They are a safe, efficient way to provide continuity of care to patients, deliver patient care faster, and limit the burden on supervising physicians. The technology is incredibly useful at this point in the pandemic, when many healthcare practices are navigating unprecedented staffing deficiencies.
In Salem, Massachusetts, it can take more than 150 days to schedule a cardiology appointment.
Reducing Appointment Wait Times
APs can use eConsults to improve patient access management. Wait times for specialty care are increasing. A recent survey by AristaMD revealed that wait times across the county are trending up in many specialties:
- Patients in Aurora, Colorado, are waiting approximately 90 days to see a cardiologist. In Salem, Massachusetts, scheduling a cardiology appointment can take more than 150 days.
- Dermatology appointments have been difficult for patients to schedule for many years. Today, a patient in Jacksonville, Florida, will wait about 70 days for an appointment to examine a suspected melanoma.
- In Huntsville and Birmingham, Alabama, patients will wait more than 100 days to see an Endocrinologist.
As a result, patient access management is now more difficult due to an overburdened and understaffed healthcare system. The use of eConsults by APs enables patients to get rapid access to specialists while providing care in the most appropriate setting possible.
Expert Support for Advanced Practitioners
APs are poised to alleviate the crisis in staffing and, with the help of eConsults, can ensure patients efficiently and effectively gain access to specialty care.
Using eConsult technology, advanced practitioners can manage patients who need specialty care, relieving the burden on providers while increasing the quality of care for patients.
Mid-level providers, including nurse practitioners and physician assistants, can use eConsults to help patients gain access to specialists, reduce wait times for specialty care, and provide game-changing support to both PCPs and specialists.
eConsults can improve the quality of patient care by:
- Reducing the amount of review required by the supervising physician.
- Providing instant access to US-based, board-certified specialists.
- Allowing advanced practitioners to get patient care advice in less than 24 hours. In most cases, advice is returned in less than 4 hours.
- Eliminating the escalation of patient care to the primary care physicians in the clinic or practice.
eConsults support physicians in another important way. They help protect a practice’s most valuable assets—the employees—from exposure and burnout.
During a time when there is a tremendous need to expedite patient care amid shrinking resources, mid-level practitioners can use eConsults to include specialty guidance in their treatment plans without the need for extensive supervision or a face-to-face specialist visit.
Efficiency is a top concern for vulnerable patients who have avoided or postponed care out of fear of contracting Covid. eConsults can accelerate care for patients waiting to see a specialist. Expediency and cost-effective treatment options are particularly important for providers operating under a value-based care payment model.
Whitepaper: eConsults Connect PCPs to On-call Specialists to Collaborate on Patient Cases
For healthcare organizations, telehealth has proven to be an effective tool to combat COVID-19 related challenges posed to the system.
It’s time to assess eConsults as a critical component of an effective telehealth strategy.