Are eConsults a Form of Telehealth?
Telehealth is the use of electronic information and technology to support and promote long-distance clinical healthcare, patient and professional health-related education, public health and health administration.* There are various types benefitting providers, healthcare organizations, and patients.
* The Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Service
Telehealth is a complete strategy incorporating multiple types of telehealth technology services acting as a complete and comprehensive solution. It includes an array of solutions that improve healthcare delivery for providers, patients and communities.
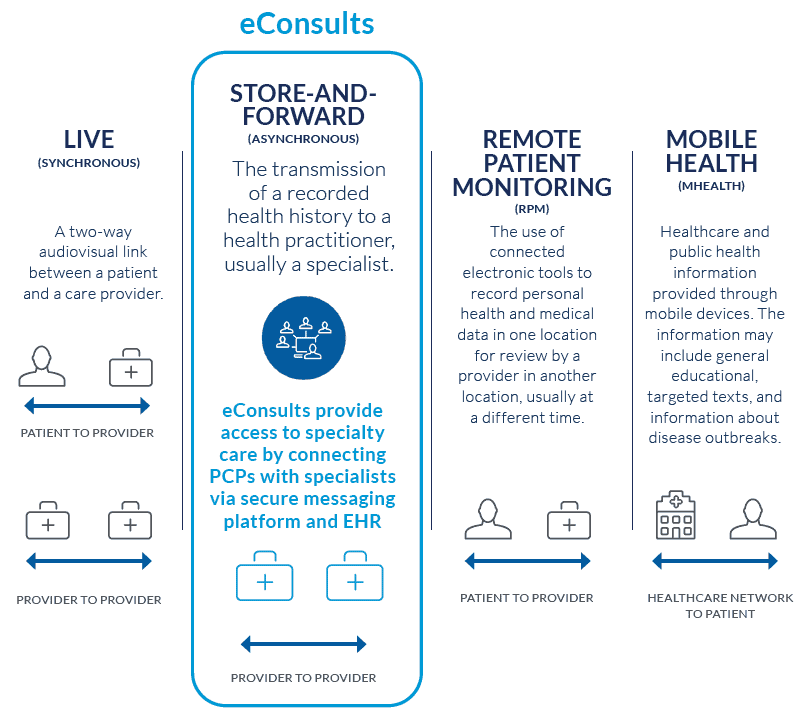
Types of Telehealth
There are several types on the market, including mHealth (or mobile health), video and audio technologies, digital photography, remote patient monitoring (RPM), and store and forward technology (commonly referred to as asynchronous) or eConsults.
These solutions can help address specialist shortages, increase patient engagement and satisfaction and enable improved provider communication, education, and satisfaction.
Live (Synchronous) Video Conferencing
Two-way audiovisual (teleconferencing) link between a patient and a care provider
Store-and-Forward Telehealth (or Asynchronous Telehealth) Technology
Documented transmission of a recorded health history to a health practitioner, usually a specialist, via secure messaging platform
Remote Patient Monitoring (RPM)
The use of connected electronic tools to record personal health and medical data in one location for review by a provider in another location, usually at a different time
Mobile Health (mHealth)
Healthcare and public health information provided through mobile devices. The information may include general educational information, targeted texts, and notifications about disease outbreaks
What are the benefits of telehealth?
Improves access to necessary care
Increases patient satisfaction and patient health outcomes
Decreases healthcare cost
Better manages “right time, right place, right provider care”
Reduces specialist and impacted physician visit wait times
Increases provider scope and satisfaction
Reduces hospital admissions and readmissions
Alleviates the effects of physician shortages
Facilitates increased patient engagement
Often reduces cost burden for patients
Learn more about our eConsult solution.
How to Get Started?
AristaMD provides an innovative store-and forward, asynchronous telehealth service. Our eConsult solution enables primary care physicians to collaborate with a national panel of top telehealth specialists on patient care plans—within 24 hours. AristaMD’s eConsult solution consistently replaces the need for more than 70% of in-person specialty visits and significantly influences care plans >90% of the time.
Empowering PCPs to treat low acuity patients with the guidance of a virtual specialist, via telehealth solution, avoids unnecessary in-person referrals and improves patient wait times while improving health system quality metrics and patient satisfaction.
With AristaMD, adopting an eConsult solution is simple and can be done quickly. Designed to seamlessly integrate into clinical workflows, the platform allows payers and providers to quickly and cost-effectively launch specialist eConsults.
Ready to get started?
