Uncompensated care drops hospital revenue, but digital health consultations by PCPs offer a proven solution to decrease uncompensated care.
Featured in Electronic Health Reporter, Healthcare Business Today, and Healthcare Business and Technology | By Chris Jaeger, AristaMD Head of ACO and Health System Strategy
Rural hospitals are facing severe challenges in maintaining operating margins, with uncompensated care being a major factor. A digital health consultations platform use in local primary care settings to improve “right time, right place, right provider care” have been shown to decrease the number of patients receiving avoidable and unnecessary care within the hospital setting, thus supporting hospital’s ability to mitigate uncompensated care.
As aligned with organizational missions, hospitals incur costs while delivering services to a diverse population of patients in need of medical attention.
Uncompensated care is an overall measure of hospital care provided for which payment was not received from the patient or payer group. It equates to the sum of a hospital’s bad debt plus the financial assistance it provides to patients, often referred to as charity care.
A hospital incurs bad debt when it cannot obtain reimbursement for care provided; this happens when patients are unable to pay their bills, but do not apply for financial assistance, or are unwilling to pay their bills.
Financial assistance includes care for which hospitals never expected to be reimbursed and care provided at a reduced cost for those in need. Hospitals, both nonprofit and for-profit, provide uncompensated care for individuals who are un- and underinsured.
These costs are a constant for hospitals, built into budgets and projections.
Thirty-seven states have adopted Medicaid expansion programs since the 2014 passage of the Affordable Care Act and Medicaid expansion. Rural areas tend to have larger proportions of low-income populations that benefit from Medicaid expansion, thus within these 37 expansion states, more vulnerable citizens have been able to benefit from expanded coverage and more access to affordable care.
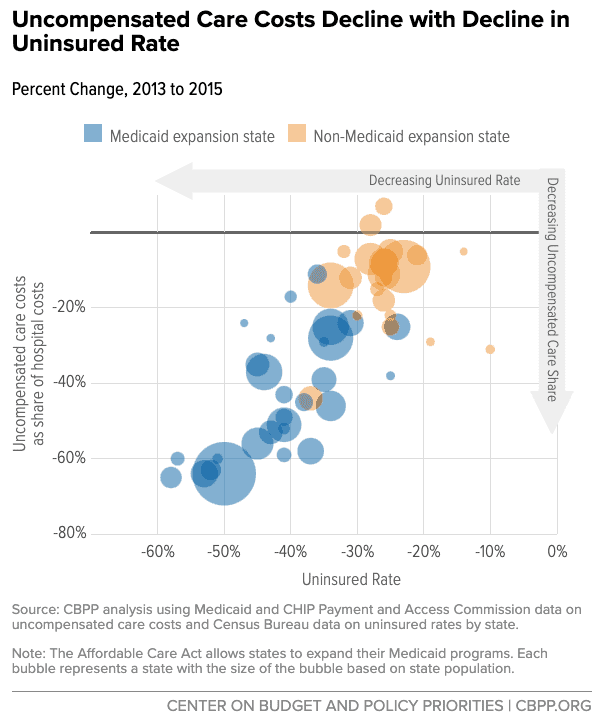
After expansion, the uninsured rate fell to a record low across all US states, though it dropped the most within expansion states. Specifically, some rural areas in states that have expanded Medicaid have seen more than a 20 percent reduction in uninsured populations.
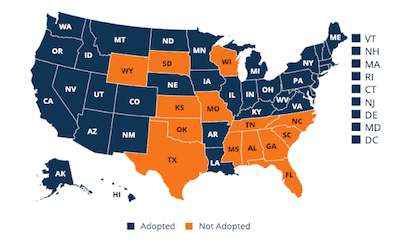
Despite the improvements within expansion states, the same impact on the rate of uninsured patients and uninsured care provided by hospitals has not carried over to states not participating in the expansion.
Recent study by the North Carolina Rural Health Research Program (NC-RHRP) at the University of North Carolina Cecil G. Sheps Center for Health Services Research (UNC-CH) showed that since 2010, 89 rural hospitals in 26 states have closed.
A majority of these closures are within states not participating in Medicare expansion. This means uncompensated care and declining margins are still causing hospitals, especially in rural areas, to close.
The availability of necessary (non-emergency) care still remains an issue for patients, especially for safety-net providers which care for a disproportionate high-utilizing portion of the patient population.
Medicaid expansion results in a reduction of both unnecessary and avoidable emergency setting care. Unnecessary qualifies as emergency department (ED) visits that could and should have been cared for in a lower-acuity setting, such as primary care.
Avoidable visits are those for worsening of chronic conditions that given the decline warrant acute intervention, but if the patient had had appropriate care in a lower-acuity setting (primary care being a prime example), the worsening would not have occurred.
Much of the uncompensated care, frequently avoidable, provided by hospitals could be prevented through timely access to necessary care, lead by primary care intervention, A report, released by Premier, found:
Six common chronic conditions accounted for 60 percent of 24 million Emergency Department (ED) visits in 2017; out of that 60%, approximately 1/3 of the visits (4.3 million) were likely preventable and could be treated in a less expensive outpatient setting.
In addition, a retrospective cohort study of the impact of a primary care intervention (including an in-hospital, free, adult clinic for poor uninsured patients on ED visit rates and emergency severity at a nonprofit hospital) provided a statistically significant correlation between primary care intervention and ED visits.
ED visit rates of new high-users post-primary care intervention were lower than preintervention high-users’ rates in the preintervention period. Uninsured high users showed similar results.
Another barrier in proactive care management is the open-looped specialty referral process, where the responsibility of obtaining specialty care relies mainly on the patient to schedule, wait, and follow through with specialist visits, in the case that specialist appointments are even available.
Amidst specialist shortages appointment wait times suffer, causing patients to wait extended periods of time or forgo necessary care, in turn often leading them to seek care within emergency settings. To better support primary care with access to resources empowering more complete patient care, community care centers are adopting telehealth platforms to increase access to timely, high-quality support.
Specifically, eConsult platforms increase access to specialist guidance from within the primary care office to improve “right time, right place, right provider” care.
This reduces unnecessary referrals and empowers primary care providers to better manage total patient care. Increased access to necessary care could strengthen primary care’s positioning as a solution to mitigate the number of patients seeking care within ED settings that is more appropriate for primary care.
eConsults are a resource that has shown to support the reduction of up to 30% of admissions and 17.1% of readmissions. Community primary care eConsult use could support for-profit hospitals in decreasing the amount of uncompensated care they are providing.

